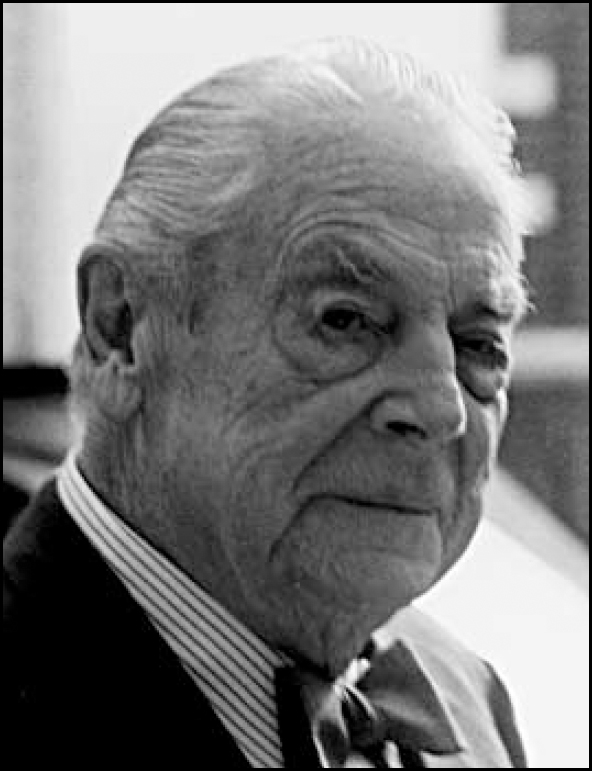
Dr Davies died of myeloid leukaemia on 13 August 2001, aged 88 years. Beresford, as he was known by all of his professional associates, was one of Cambridge's most distinguished psychiatrists, a statesman-like figure and a legend among his colleagues and patients. He was an indefatigable worker and he continued to see a few patients until shortly before his death.
Edward was born in Liverpool. He went to Oundle and there excelled in shooting. After school he went up to Clare College, Cambridge, in 1931 to read Medical Sciences Tripos. During his first year at Cambridge he developed pneumonia that was slow to resolve. It was decided that he would be helped by a period of mountain air and was sent to Norway to convalesce. While there he was invited to attend a wedding; this was a very important occasion in his life for there he met Hendriette Fuglesang, the girl who eventually became his wife.
Back in Cambridge he took a full part in the life of his college and the university. He continued to shoot and he took up fencing. He became fascinated by the theatre and regularly wrote reviews for the newspapers. He took his BA in 1934 and went to the Middlesex Hospital to continue his medical studies. He married Hendriette soon after he qualified. War was looming and, after a brief period as a junior psychiatrist at the Towers Hospital in Leicester, he volunteered for the Royal Air Force.
With his natural flair for languages he had picked up Norwegian very quickly as the result of his days in Norway and from Hendriette; he soon became fluent in the language. So equipped he was posted to a Norwegian Spitfire unit based variously in North Weald, Manston and Ipswich. Always keen on flying, he undertook pilot training but was frustrated by the fact that, as a medical officer, he was never allowed to fly himself operationally. However, he did fly as an RAF observer over the Battle of the Falaise. He wrote a major part of the Manual of Air Sea Rescue and, later, the Medical History of the RAF. He reached the rank of Wing Commander, and for a time, served on the staff at the Air Ministry. He went to France within a few days of the invasion and was in Paris before it was liberated.
Having observed the effect of battle stress upon the men with whom he had served, his earlier intention to become a psychiatrist was stronger than ever, and after leaving the Royal Air Force he went back to the Towers Hospital for 2 years. Then followed a year at Banstead Hospital, near Espom, Surrey, and at St Stephen's Hospital in Chelsea. He was then ready to seek a consultant post and he was fortunate enough to be accepted for a job in Cambridge. However, he soon came face to face with the fact that there were considerable problems in the Cambridge psychiatric service. Psychiatry there was entirely centred upon Fulbourn Hospital, a large traditional mental hospital that had been built in the mid-19th century some 4 miles outside the town and was still run along old fashioned lines. The patients were treated humanely but therapeutic methods were hopelessly outdated and there were major difficulties with the then medical superintendent, essentially a decent man but one whose influence was disruptive and opposed to change. Together with two other young and newly appointed colleagues, Edward pressed for a re-organisation of the service. He was totally opposed to the idea that Fulbourn should remain out of sight and out of mind, completely detached from the main general hospital. He insisted that he should be given out-patient facilities at Addenbrooke's and was subsequently the first consultant psychiatrist appointed specifically to that hospital. Like all psychiatrists of his generation he was enormously excited by the discovery and development of the neuroleptic drugs, providing, as they did, a first significant input into the treatment of schizophrenia. But when the anti-depressant drugs appeared in 1960 he had the foresight to recognise that these would have an equally far reaching impact upon the care of the mentally ill. In that same year he organised an international conference in Cambridge, one of the first of its kind, to look at all aspects of anti-depressant treatment. His approach to his patients was essentially electic. He used psychotropic medication when it was indicated, but he was also a well-trained and skilful psychotherapist. He was sensitive and extremely kind to his patients and he was held in the highest esteem by them. He developed a flourishing private practice but it was not widely known that he was exceptionally generous to many of those patients who came to his rooms. Doctors, nurses and members of the cloth were never charged fees and people whom he realised were ‘hard up’ paid only minimal amounts. He had always been interested in the use of lithium in the treatment of affective illness and together with a patient who suffered from bipolar affective disorder, he started the Lithium Club, open to all who needed to take lithium. Originally a local initiative, this became a national charity, intended to provide support to patients and their relatives not only from the Cambridge area but from all over the country. Another of his particular interests and areas of expertise was in the care of patients with alcoholism.
Edward passed the DPM in 1940 at the time of joining the RAF and he gained his MD in 1949, this based upon his research and thesis into the effects of electroconvulsive therapy. He was a Founder member of the Royal College of Psychiatrists and he was elected to the Fellowship in 1971. He was an associate lecturer at the University of Cambridge.
Hendriette died in 1993. Her death, after 55 years of marriage, hit him very hard. By good fortune, after a few lonely years, he married Barbara Simpson, herself a doctor's widow and an old friend of the family. She gave him an entirely new lease of life. Those who knew him well watched him flourish again. He is survived by his three children.





eLetters
No eLetters have been published for this article.